This article presents an FAQ on recurrent early prenancy loss where common causes such as age, genetics, anatomic, and hormonal problems are explained.
Having an early pregnancy loss (EPL), also known as miscarriage, can be quite distressing for both women and their partners. However, when it happens yet again, it can be very devastating and understandably, make you feel quite low, sad or angry.
It is not surprising as a result, many women resort to googling on the internet, seeking answers to why has it happened and whether anything can be done to prevent it from happening again and to achieve a live birth in next pregnancy.
We have made an attempt to help you by creating a frequently asked questions (FAQs) list along with some reliable resources.
FAQ about recurrent early pregnancy loss (miscarriage)
Loss of a pregnancy usually up to 12 weeks gestation (approximately 3 months pregnant) is referred to as an early pregnancy loss or miscarriage. However, when a woman loses a pregnancy 2-3 times or more, then it is referred to as recurrent miscarriage.
There is no consensus across different countries as to how many losses would constitute to recurrent EPL. In the UK, national bodies refer to three or more consecutive losses as recurrent EPL whereas in the USA and the rest of Europe, the criteria states 2 or more loss. It is further complicated by the fact that there is no agreement whether these should be with same partner or in successive pregnancies without any live birth in between. In addition, pregnancy losses due to several specific reasons are usually not accounted for in the criteria. These include as loss due to an ectopic pregnancy (a pregnancy located outside the womb, usually in the fallopian tube), a molar pregnancy (usually referred to as an overgrowth of pregnancy tissue without any obvious presence of a live fetus within) or a biochemical pregnancies (i.e a pregnancy lost following a positive pregnancy test before further tests such as scan can be done).
Although 1 in 4 pregnancies routinely may end up in a miscarriage, recurrent early pregnancy loss happens less frequently. It is reported that 1 in a 100 women would experience recurrent early pregnancy loss.
There is evidence that poor health status can lead to poor pregnancy outcomes, therefore it is recommended that you and your partner ensure you are in best of your health and follow a healthy diet and lifestyle to ensure optimising a chance of a pregnancy. Smoking, excess weight etc can be detrimental to a pregnancy outcome and hence if you are thinking of trying again, please follow a healthy advice. Further information is available here.
There are some known and possible causes attributed to recurring early pregnancy losses. However, in almost half of the women tested for recurrent pregnancy loss, there will be no cause identified. This is often referred to as unexplained.
If you or your partner has experienced recurrent early pregnancy loss then you should seek expert opinion from a specialist doctor in the field.

Common causes of recurrent early pregnancy loss
The older a woman is, higher the chance of her losing a pregnancy. The risk starts to increase from mid-30s rapidly.
Although, there are emerging reports to state that a man’s age (if over 40) may also have an indirect effect on conferring an increased risk of miscarriage, one needs to bear in mind that the evidence for this is not strong currently
It is not uncommon to experience a pregnancy loss due to abnormality in the genetic makeup of the pregnancy itself. This does not mean though that you or your partner carry a genetic mutation that can be passed on and result in pregnancy losses, but rather that there has been a problem with the way that the sperm and egg that went into making the pregnancy formed.
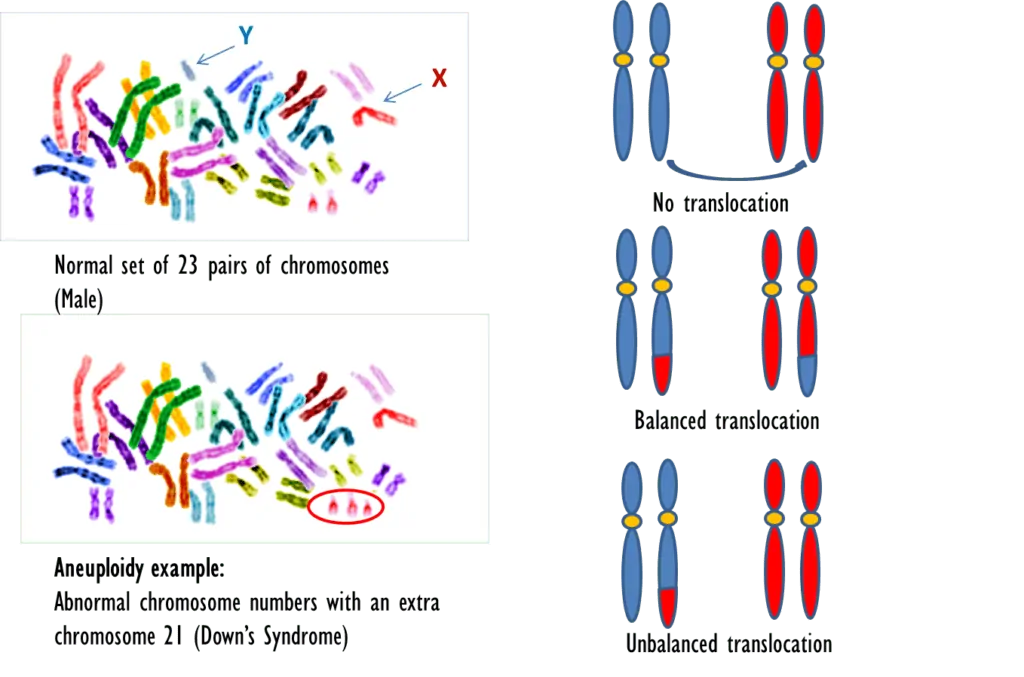
Our DNA is made up of pairs of chromosomes that carry hereditary information in the form of genes. We inherit half of our DNA from our mother and the other half from the father. One of the common chromosome abnormalities that result in a miscarriage is having an extra chromosome. This can be linked to the age of the mother, as the eggs of older women are of lower quality. The older the woman at the time of conceiving, the more likely there is of having a problem with the chromosomes as the dividing egg does not halve the number of chromosomes equally. This in turn results in the embryo either acquiring extra chromosome numbers or having less than the normal set of chromosomes. This type of chromosomal abnormality is collectively referred to as aneuploidy.
Almost half of miscarriages occur due to these types of chromosomal abnormalities of the embryo. This occurs randomly and is not an inherited problem.
However, if on genetic testing it is noted that there is a translocation, meaning that parts of the chromosomes have been swapped around and are now on the wrong chromosomes, places then this may result in recurrent pregnancy loss. This is less common (3-5%). If all genes post cross-over are present, it is known as balanced translocation but if parts of chromosomes are either doubled up or missing altogether, then it would result in what is called an unbalanced translocation. If this is picked up then you and your partner may be offered a genetic testing of your own DNA to see whether you have the genetic condition.
The figure below explains the difference between aneuploidy and translocation type of genetic abnormalities.
Genetic causes: Aneuploidy vs translocation
Your doctor will send a sample from the pregnancy loss for genetic testing to confirm whether there was any known genetic cause. If it is attributed to translocation then your doctor may invite you and your partner for a blood test for genetic testing of your DNA. Although it is usually done by taking a blood sample, it can also be done by testing other samples such as saliva or swab from mouth.
If the test shows a genetic condition, your doctor may advise referral to a genetics specialist to discuss this further.
Most often, if someone is known to have a balanced translocation themselves, it is unlikely to have significant health effects on your own well-being. Your doctor and the genetics specialist will explain that further.
The genetics specialist will discuss the chance of a live birth, risk of transmitting it and options to avoid it being inherited.
One of the options that may be relevant to discuss is the possibility of doing IVF based technique called preimplantation genetic testing to select the embryos that are healthy to transfer into the womb to achieve a pregnancy.
Please note this is not an option for all and will depend on several factors which your doctor would explore and if relevant refer you to a fertility specialist for an in-depth discussion.
Blood Clotting problems
There are several blood disorders or conditions but the only one known to be associated with recurrent early pregnancy loss is known as Antiphospholipid syndrome (APS) which is an autoimmune condition that make your blood more sticky than normal. This is due to some abnormal antibodies a person acquires but is not born with it.
It results from your immune system producing antibodies that attack proteins attached to fat cells called phospholipids, thus making the blood more prone to clot. The exact mechanism of why it happens is not known. Your doctor would assess you for these antibodies such as lupus anticoagulant and anticardiolipin antibodies.
These antibodies can make the blood cells sticky so that it forms tiny clots (microvascular thrombosis) in the blood vessels feeding the growing pregnancy. This results in reduced blood circulation to the fétus and may thus cause a pregnancy to be lost.
You doctor would take a small blood sample from you to test whether your blood contains these antibodies or not. It is not uncommon to test positive for the antibodies when you don’t have APS and your doctor may recommend testing you again to confirm that the first result was correct.
Your doctor will speak to you about various blood thinning options for your next pregnancy. Please see additional information resources which give more details on this.
Medical research does not support that inherited sticky blood conditions such as Factor V Leiden gene mutation, Protein S or Protein C deficiency contribute to early pregnancy loss. However, they are associated with later pregnancy problems including late miscarriages or having a small baby.
Problems with the anatomy of the womb
This condition could be since birth if related to shape of the womb or one developed later due to some pathology within the cavity.
In some women, there is a possibility that they were born with an abnormality of the womb. If the shape of the womb is not normal then it may result in loss of pregnancy. One such abnormality in the shape of the womb is the presence of a septum i.e. a thin curtain separating the cavity of the womb.
Sometimes the shape of the womb is normal but women may have some other problem in the womb cavity such as a benign fibroid or a polyp. Occasionally, there may be scar tissue within the cavity caused by previous surgery, infection or trauma. This is called ‘Asherman syndrome’ or ‘synechiae’.Sometimes, a woman may have a weak neck of the womb, referred to as an ‘incompetent cervix’. This does not cause early pregnancy loss but may result in the loss of pregnancy in later gestation or preterm birth.


Your doctor may arrange a detailed (3D) internal pelvic ultrasound scan to look at the shape of the womb and the rest of pelvic anatomy such as ovaries. In some cases, it may be necessary to do a small procedure called hysteroscopy where a camera is passed through the neck of the womb to look inside the cavity.
Your doctor will advise you further whether you need any surgery to correct the problem and the associated risks. Most of the relevant surgery will be done internally without the need of making any cut on the tummy. The doctor will also discuss whether the evidence shows that surgery would improve your chance of reducing future pregnancy loss and having a baby.
Hormone causes
Some of the other causes that may need exploring are any hormone disturbances that may attribute to pregnancy losses.
Your doctor will talk to you about these hormone disturbances such as polycystic ovarian syndrome (PCOS), thyroid problems or diabetes. These are only looked into if there is any history or symptoms to suspect this.
A lack of adequate progesterone hormone to support the pregnancy may also be one of the reasons, but it is not clear whether it is the cause of RM or just something that is seen when a pregnancy is already failing.
Your doctor will offer relevant blood tests if indicated to diagnose any hormone problem. If any hormone disturbance such as a thyroid problem or diabetes is identified, then your doctor would refer you to a specialist for further advice.
Please see below recent research findings on the role of progesterone support.
What about natural killer cells?
It is believed that the lining of the womb have some cells that may prevent the pregnancy from continuing by attacking the pregnancy. These are referred to as Natural Killer cells and are part of the immune system. There is also a different type of Natural Killer cells present in blood. There is no robust evidence to recommend that Natural Killer cells be tested or that they cause recurrent EPL. However, some centres offer these tests despite the lack of evidence.
At present, strong evidence is lacking that links sperm DNA damage to recurrent early pregnancy loss and most professional bodies do not recommend offering this test.
If all the tests offered to you or your partner have come back clear and there is no known explanation for your pregnancy loss, the doctor would offer you an early pregnancy scan appointment in your future pregnancy. Please also be sure to take folic acid and vitamin D supplements.
Despite having had recurrent early pregnancy losses, it is not all doom and gloom. There is still a high chance of having an ongoing pregnancy and successful live birth.
The prediction chart as shown below by Brigham et al (Human Reproduction, 1999) may be a helpful guide to refer to. The guide is adapted from Brigham et al, Human Reproduction, 1999.
Progesterone therapy: The PROMISE trial (Coomarasamy et al, NEJM, 2015) found that there was no higher chance of having a baby if progesterone was given during early pregnancy, for women who have had recurrent miscarriage. However, a separate study called the PRISM trial (Coomarasamy et al, NEJM, 2019 & AJOG, 2020) did show that a subgroup of women who have had previous EPL and had fresh bleeding in the current pregnancy (threatened miscarriage) may benefit from progesterone supplements. Please discuss this further with your doctor.
Thyroxine use: The TABLET trial (Dhillon-Smith et al, NEJM, 2019) did not show any improvement in chance of having a baby by giving thyroxine tablets to women who had thyroid autoantibodies but who had normal thyroid function. Hence, this is not a recommended treatment if you just have antibodies but do not have a thyroid problem per se.
Immunotherapy: The RESPONSE trial (Eapen et al, Hum Rep, 2019) did not show that women who had suffered from unexplained recurrent miscarriages and were given a synthetic protein (GCF/NT 100) during their early pregnancy, were more likely to have a live birth.
There is no evidence to support role of immunotherapy or steroids for treating recurrent miscarriages.
If you are keen to take part in any research study, your doctor will be the best port of call to give you information about current studies.
Some of the resources listed below are reliable sources of information and hopefully will guide you through this difficult and emotional journey.
- https://www.miscarriageassociation.org.uk/
- https://www.tommys.org/pregnancy-information/pregnancy-complications/baby-loss/miscarriage-information-and-support
- https://www.rcog.org.uk/globalassets/documents/patients/patient-information-leaflets/pregnancy/pi-recurrent-and-late-miscarriage—tests-and-treatment-of-couples.pdf
- https://www.eshre.eu/Guidelines-and-Legal/Guidelines/Recurrent-pregnancy-loss.aspx
- https://www.asrm.org/topics/topics-index/miscarriage-or-recurrent-pregnancy-loss/